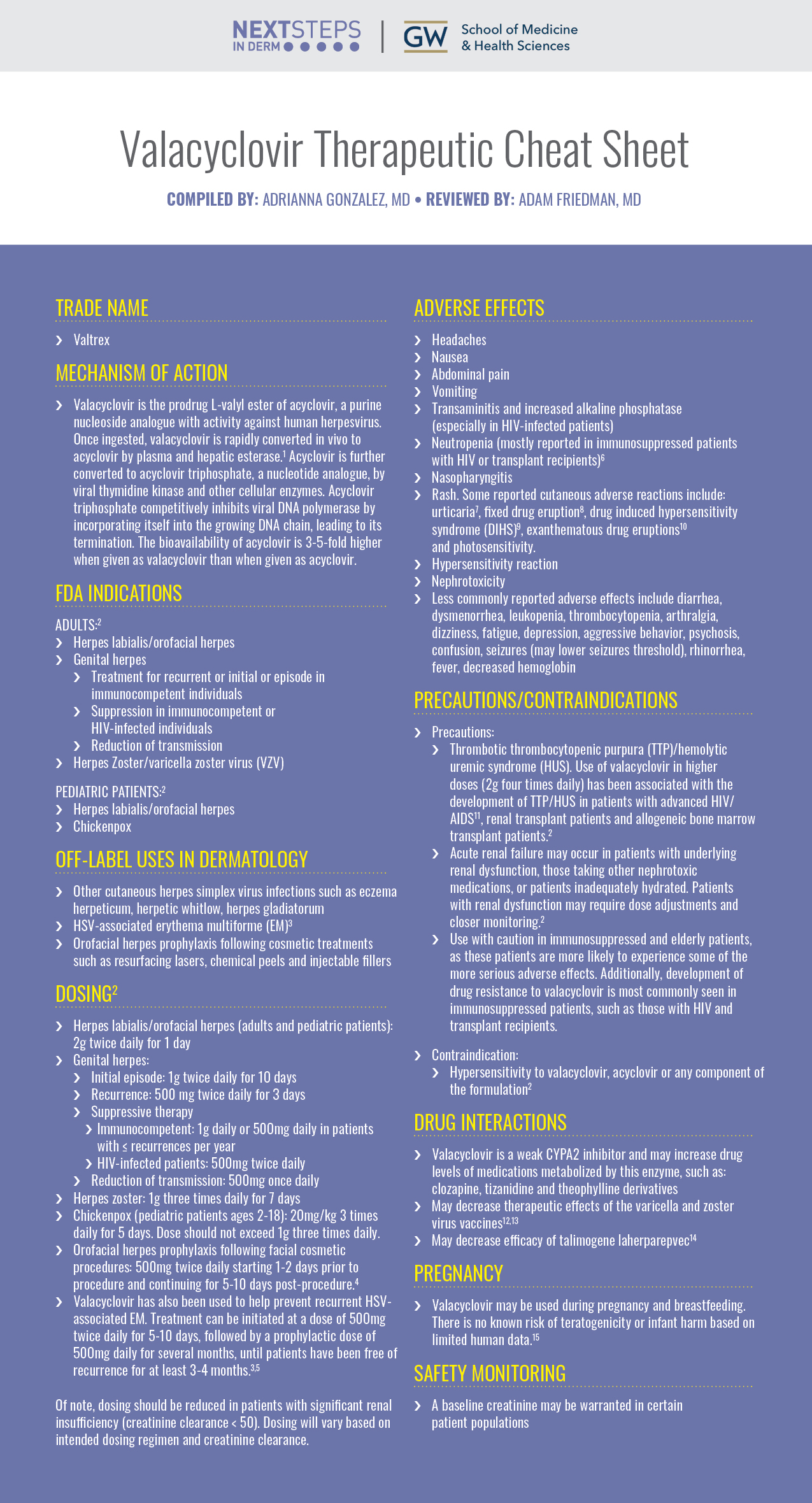
Valacyclovir, a medication often prescribed for herpes simplex virus (HSV) infections, tackles both oral and genital herpes effectively. It reduces the duration and severity of outbreaks, minimizing painful symptoms like blisters and sores. This antiviral medication works by inhibiting viral DNA replication, thus curbing the virus’s ability to spread.
Beyond herpes, Valacyclovir demonstrates efficacy against shingles (herpes zoster). By targeting the varicella-zoster virus (VZV), responsible for both chickenpox and shingles, it helps shorten the duration of the painful rash and associated nerve pain. Early treatment is key for minimizing complications.
Furthermore, Valacyclovir finds use in preventing recurrences of both herpes simplex and herpes zoster. Regular, preventative use, as prescribed by a physician, significantly lowers the frequency and severity of future outbreaks. Always consult your doctor before starting any preventative treatment regimen.
Important Note: Valacyclovir is a prescription medication. Always follow your doctor’s instructions meticulously regarding dosage and duration of treatment. Do not self-medicate. Discuss potential side effects and interactions with other medications with your healthcare provider before starting treatment.
- What Valacyclovir is Prescribed For
- Specific Uses and Dosages
- Genital Herpes (HSV-2) Treatment
- Dosage and Administration
- Managing Outbreaks
- Suppressive Therapy
- Potential Side Effects
- Important Considerations
- Alternative Treatments
- Genital Herpes (HSV-2) Suppression
- Dosage and Administration
- Important Considerations
- Oral Herpes (HSV-1) Treatment
- Dosage and Administration
- Managing Symptoms
- When to Seek Medical Attention
- A Note on Prevention
- Chickenpox (Varicella-zoster virus) Treatment
- Managing Symptoms
- When to Seek Medical Attention
- Shingles (Herpes Zoster) Treatment
- Prevention of Herpes Transmission
- Post-Herpetic Neuralgia (PHN) Management
- Pharmacological Options
- Non-Pharmacological Strategies
- Important Considerations
- Follow-up Care
What Valacyclovir is Prescribed For
Valacyclovir treats herpes simplex virus (HSV) infections, including cold sores (oral herpes) and genital herpes. It also effectively manages herpes zoster (shingles), a painful rash caused by the varicella-zoster virus (VZV).
Specific Uses and Dosages
For cold sores, doctors often prescribe valacyclovir to shorten the duration and severity of outbreaks. Genital herpes treatment aims to reduce the frequency and severity of recurrences. Shingles treatment with valacyclovir lessens the duration and intensity of the rash and associated pain. Your doctor determines the appropriate dosage based on your specific condition and medical history. Always follow your physician’s instructions carefully. Remember that valacyclovir is an antiviral medication; it doesn’t cure herpes but helps manage symptoms.
Beyond these primary uses, valacyclovir might be prescribed for other conditions related to these viruses, such as the prevention of transmission in individuals with genital herpes or the management of complications arising from these infections. These applications are usually based on individual patient assessment and medical advice.
Genital Herpes (HSV-2) Treatment
Valacyclovir is a common antiviral medication prescribed to manage genital herpes. It doesn’t cure the virus, but it significantly reduces outbreaks.
Treatment aims to lessen the severity and frequency of symptoms. This includes reducing the duration and pain of sores, and decreasing viral shedding (the period when the virus is contagious).
Dosage and Administration
Your doctor will determine the appropriate dosage based on your individual needs. Typically, treatment involves taking valacyclovir daily, even without symptoms, to suppress outbreaks. The frequency of dosing varies. Always follow your doctor’s instructions precisely.
Managing Outbreaks
During an outbreak, your doctor might recommend a higher dose of valacyclovir for a short period to quickly alleviate symptoms. This helps to shorten the duration and reduce discomfort.
Suppressive Therapy
Long-term suppressive therapy with valacyclovir is a viable option for many. It reduces the likelihood of future outbreaks and minimizes the risk of transmission.
Potential Side Effects
While generally well-tolerated, valacyclovir can cause side effects such as headache, nausea, and fatigue. Discuss any concerns with your doctor.
Important Considerations
| Aspect | Details |
|---|---|
| Transmission | Genital herpes is highly contagious; practicing safe sex is paramount. |
| Condoms | Condoms offer some protection, but they don’t guarantee complete prevention of transmission. |
| Regular Checkups | Regular visits to your doctor for monitoring are recommended. |
Alternative Treatments
Acyclovir and famciclovir are alternative antiviral medications that may be used. Your doctor will help you determine the best option for your situation.
Genital Herpes (HSV-2) Suppression
Valacyclovir helps manage genital herpes outbreaks. Daily suppressive therapy significantly reduces the frequency and severity of outbreaks. This means fewer painful sores and less virus shedding.
Dosage and Administration
Your doctor will determine the appropriate dosage, typically a daily dose of valacyclovir. Consistent daily use is key for optimal suppression. Missing doses reduces effectiveness.
Remember, valacyclovir suppresses, but doesn’t cure, herpes. Consistent medication use is necessary for ongoing management. Regular follow-up appointments with your doctor are recommended to monitor treatment success and adjust the dosage if needed. Open communication with your healthcare provider about any concerns is vital for the best outcomes. It’s also crucial to practice safe sex to prevent transmission to partners.
Important Considerations
Valacyclovir can interact with other medications. Inform your doctor of all medications you are taking, including over-the-counter drugs and supplements. Potential side effects, while generally mild, include headache, nausea, and fatigue. Report any significant side effects to your physician immediately.
Oral Herpes (HSV-1) Treatment
Valacyclovir is a common prescription for oral herpes. It reduces the duration and severity of outbreaks. The typical dosage is 1 gram twice daily for one day, starting at the first sign of an outbreak.
Dosage and Administration
Always follow your doctor’s instructions precisely. Failure to adhere to the prescribed dosage may lead to treatment failure. For recurrent outbreaks, your doctor might prescribe a lower daily maintenance dose to prevent future occurrences. This preventative dose helps keep the virus under control.
Managing Symptoms
While valacyclovir targets the virus, you can manage symptoms with over-the-counter remedies. Applying a topical anesthetic cream can numb the painful sores. Keeping the area clean and dry helps prevent secondary infection. Avoid touching the sores and sharing utensils or lip products to prevent spreading the virus.
When to Seek Medical Attention
Seek immediate medical advice if your symptoms worsen, spread significantly, or you experience other concerning symptoms like fever or swollen lymph nodes. Severe or persistent outbreaks may require further evaluation and a different treatment plan. Regular follow-up appointments with your doctor ensure proper management of the condition.
A Note on Prevention
Remember, while valacyclovir treats outbreaks, it doesn’t cure HSV-1. Practicing good hygiene and avoiding close contact with others during an outbreak are key to preventing transmission.
Chickenpox (Varicella-zoster virus) Treatment
Valacyclovir is one treatment option for chickenpox, particularly in adults or individuals at higher risk of complications. It helps shorten the duration of the illness and reduce the number of lesions.
Managing Symptoms
Beyond antiviral medication, focus on symptom management. Calamine lotion soothes itchy skin. Oatmeal baths can provide similar relief. Over-the-counter pain relievers like acetaminophen or ibuprofen can manage fever and discomfort. Keep fingernails short to minimize scratching and prevent secondary infections. Hydration is key; encourage plenty of fluids.
When to Seek Medical Attention
While chickenpox usually resolves on its own, seek medical advice if symptoms are severe, if complications arise (such as bacterial skin infections or pneumonia), or if the rash spreads rapidly. Adults and immunocompromised individuals should always consult a doctor for treatment.
Shingles (Herpes Zoster) Treatment
Valacyclovir can significantly reduce the duration and severity of shingles. Doctors often prescribe it within 72 hours of the rash appearing for optimal results. This antiviral medication works by targeting the varicella-zoster virus, responsible for both chickenpox and shingles.
Treatment typically lasts for a week. Your doctor will determine the correct dosage based on your health status. Remember to complete the full course, even if symptoms improve. Stopping early might lead to recurrence or complications.
Beyond valacyclovir, pain management is a key aspect of shingles treatment. Your physician might recommend over-the-counter pain relievers like ibuprofen or acetaminophen, or prescribe stronger medications if needed. Prescription topical creams can alleviate itching and pain directly on the affected skin.
Important Note: While valacyclovir effectively manages shingles, it doesn’t prevent it entirely. The shingles vaccine offers significant protection, especially for individuals over 50. Discuss vaccination options with your healthcare provider to minimize your risk.
Potential Side Effects: Common side effects include nausea, headache, and diarrhea. These are usually mild and temporary. Report any severe or persistent side effects to your doctor immediately.
Prevention of Herpes Transmission
Preventing herpes transmission requires consistent effort and understanding. Focus on these key areas:
- Avoid contact during outbreaks: Herpes is most contagious when sores are present. Refrain from any skin-to-skin contact, including sexual activity, during these periods. This significantly reduces transmission risk.
- Safe sex practices: Condoms offer some protection, but they don’t completely eliminate the risk as herpes can spread through skin-to-skin contact outside the condom’s coverage area. Open communication with partners about herpes status is paramount.
- Good hygiene: Frequent handwashing, especially after touching an affected area, prevents accidental spread. Avoid touching your eyes or other mucous membranes after touching a sore.
- Medication adherence: Valacyclovir and other antiviral medications can reduce the frequency and severity of outbreaks, thereby lowering the risk of transmission. Take medication as prescribed.
- Know your status: Regular testing helps identify herpes early, allowing for prompt management and reducing the chance of spreading the virus.
These strategies, used together, create a robust approach to herpes prevention. Remember, consistent action is more effective than sporadic efforts.
- Regular checkups with your healthcare provider will help monitor your condition and adjust your treatment plan as needed.
- Education is key. Learn about herpes transmission and prevention to make informed decisions about your health and relationships.
Post-Herpetic Neuralgia (PHN) Management
Valacyclovir can help reduce the duration and severity of PHN, but it’s not always sufficient. A multi-pronged approach is often needed.
Pharmacological Options
- Topical treatments: Lidocaine patches or creams can provide localized pain relief. Apply as directed.
- Oral medications: Besides valacyclovir, gabapentinoids (like gabapentin or pregabalin) and tricyclic antidepressants (like amitriptyline or nortriptyline) are frequently prescribed. Dosage varies based on individual needs and should be determined by a physician.
- Opioids: For severe, intractable pain, your doctor may consider opioids, but they’re generally reserved for short-term use due to potential side effects.
Non-Pharmacological Strategies
These methods complement medication, improving overall management:
- Physical therapy: Gentle exercises and stretches can improve mobility and reduce pain. A physical therapist can create a personalized plan.
- Transcutaneous electrical nerve stimulation (TENS): A TENS unit delivers mild electrical impulses to the affected area, potentially blocking pain signals.
- Cognitive behavioral therapy (CBT): CBT helps manage the psychological impact of chronic pain, improving coping mechanisms and reducing stress.
- Acupuncture: Some individuals find relief through acupuncture, though more research is needed.
Important Considerations
Follow-up Care
Regular check-ups with your doctor are crucial to monitor treatment efficacy, adjust medication as needed, and address any emerging complications.
Remember, PHN management is individual. Work closely with your healthcare provider to develop a tailored plan that best suits your needs and experiences.